Monday, February 22, 2010
SPORTS INJURIES: RUNNERS KNEE
What is Iliotibial Band Syndrome?
Iliotibial band syndrome is often referred to by other names, most commonly, runners knee and Iliotibial band friction syndrome, sometimes shortened to ITBS or ITBFS. All of these names refer to the same condition.
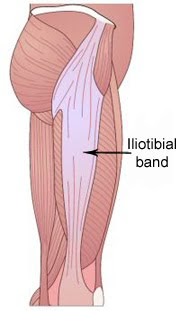
The Iliotibial band is a sheath of thick, fibrous connective tissue which attaches at the top to both the iliac crest (hip bone) and the Tensor fascia latae muscle. It then runs down the outside of the thigh and inserts into the outer surface of the Tibia (shin bone). Its purpose is to extend the knee joint (straighten it) as well as to abduct the hip (move it out sideways).
As the ITB passes over the lateral epicondyle of the femur (bony part on the outside of the knee) it is prone to friction. At an angle of approximately 20-30 degrees the IT band flicks across the lateral epicondyle. When the knee is being straightened it flicks in front of the epicondyle and when it is bent, it flicks back behind.
Iliotibial band syndrome is common in runners as 20-30 degrees is the approximate angle at the knee when the foot strikes the ground during running. In persons who run regularly this may lead to irritation of the ITB commonly known as iliotibial band friction syndrome.
Signs and Symptoms of Iliotibial Band Syndrome:
Pain on the outside of the knee (at or around the lateral epicondyle of the femur).
Tightness in the iliotibial band
Pain normally aggravated by running, particularly downhill.
Pain during flexion or extension of the knee, made worse by pressing in at the side of
the knee over the sore part.
Weakness in hip abduction.
Tender trigger points in the gluteal area may also be present.
What can the athlete do to prevent Runners knee?
Rest. Avoid painful stimuli, for example downhill running.
Apply cold therapy or ice to reduce any inflammation.
Stretch the Iliotibial band after training.
Self massage techniques can also be very helpful in correcting excessive ITB tightness.
See a sports injury specialist.
A sports injury specialist or clinician may:
Perform soft tissue or deep friction massage.
Prescribe anti-inflammatory medication such as NSAID’s e.g. Ibuprofen.
Use Myofascial release techniques which have been shown to be highly effective.
Perform dry-needling techniques.
Outline a rehabilitation strategy which may include stretches and exercises to
strengthen the hip abductors.
Use electrotherapeutic treatment techniques such as TENS or ultrasound to reduce
pain and inflammation.
In acute or prolonged cases a corticosteroid injection into the site of irritation may
provide pain relief.
What causes IT band syndrome?
Certain factors may make you more susceptible to developing iliotibial band syndrome:
A naturally tight or wide IT band
Weak hip muscles such as gluteus medius
Trigger points within the IT band and gluteal muscles
Overpronation
Overuse
Excessive hill running
Running on a cambered surface
Leg length difference
Most of these factors can be addressed through changes to your training programme, the use of insoles or heel pads and a thorough rehabilitation programme. Iliotibial band friction syndrome may require long-term rehabilitation and frequent Iliotibial band stretches should be maintained even after symptoms cease.
Assessment
Assessment of any injury should include questions concerning the patients general health, previous injuries and current injury. The aim of these questions is to determine which structure may be causing the pain and what treatment is appropriate.The therapist will then perform a physical assessment to help determine which structures are causing the pain and what might have contributed to the development of the injury.
1. Palpation of the Iliotibial band
The therapist will feel up and down the length of the IT band, assessing its general tension and feeling for any tight spots. They will also be looking for tender areas around the outer knee.
2. Obers Test
Obers test is used to assess IT band tightness. The patient is in a side-lying position, with the leg to be tested on top. The therapist will stabilise the pelvis with one hand, whilst they extend the hip with the other. They will then allow the hip to fall down towards the table (abduction). A positive result is noted if the leg moves down less than 10 degrees from horizontal.
As well as these very specific tests, the therapist will probably also look at the range of motion at the hip and knee joints. This will demonstrate how tight the surrounding muscles are, such as the hamstrings, quadriceps and gluteals. These muscles are commonly tight in cases of ITB syndrome.
The therapist should also observe the patient when standing and walking to check if they overpronate.
Iliotibial band syndrome is often referred to by other names, most commonly, runners knee and Iliotibial band friction syndrome, sometimes shortened to ITBS or ITBFS. All of these names refer to the same condition.
The Iliotibial band is a sheath of thick, fibrous connective tissue which attaches at the top to both the iliac crest (hip bone) and the Tensor fascia latae muscle. It then runs down the outside of the thigh and inserts into the outer surface of the Tibia (shin bone). Its purpose is to extend the knee joint (straighten it) as well as to abduct the hip (move it out sideways).
As the ITB passes over the lateral epicondyle of the femur (bony part on the outside of the knee) it is prone to friction. At an angle of approximately 20-30 degrees the IT band flicks across the lateral epicondyle. When the knee is being straightened it flicks in front of the epicondyle and when it is bent, it flicks back behind.
Iliotibial band syndrome is common in runners as 20-30 degrees is the approximate angle at the knee when the foot strikes the ground during running. In persons who run regularly this may lead to irritation of the ITB commonly known as iliotibial band friction syndrome.
Signs and Symptoms of Iliotibial Band Syndrome:
Pain on the outside of the knee (at or around the lateral epicondyle of the femur).
Tightness in the iliotibial band
Pain normally aggravated by running, particularly downhill.
Pain during flexion or extension of the knee, made worse by pressing in at the side of
the knee over the sore part.
Weakness in hip abduction.
Tender trigger points in the gluteal area may also be present.
What can the athlete do to prevent Runners knee?
Rest. Avoid painful stimuli, for example downhill running.
Apply cold therapy or ice to reduce any inflammation.
Stretch the Iliotibial band after training.
Self massage techniques can also be very helpful in correcting excessive ITB tightness.
See a sports injury specialist.
A sports injury specialist or clinician may:
Perform soft tissue or deep friction massage.
Prescribe anti-inflammatory medication such as NSAID’s e.g. Ibuprofen.
Use Myofascial release techniques which have been shown to be highly effective.
Perform dry-needling techniques.
Outline a rehabilitation strategy which may include stretches and exercises to
strengthen the hip abductors.
Use electrotherapeutic treatment techniques such as TENS or ultrasound to reduce
pain and inflammation.
In acute or prolonged cases a corticosteroid injection into the site of irritation may
provide pain relief.
What causes IT band syndrome?
Certain factors may make you more susceptible to developing iliotibial band syndrome:
A naturally tight or wide IT band
Weak hip muscles such as gluteus medius
Trigger points within the IT band and gluteal muscles
Overpronation
Overuse
Excessive hill running
Running on a cambered surface
Leg length difference
Most of these factors can be addressed through changes to your training programme, the use of insoles or heel pads and a thorough rehabilitation programme. Iliotibial band friction syndrome may require long-term rehabilitation and frequent Iliotibial band stretches should be maintained even after symptoms cease.
Assessment
Assessment of any injury should include questions concerning the patients general health, previous injuries and current injury. The aim of these questions is to determine which structure may be causing the pain and what treatment is appropriate.The therapist will then perform a physical assessment to help determine which structures are causing the pain and what might have contributed to the development of the injury.
1. Palpation of the Iliotibial band
The therapist will feel up and down the length of the IT band, assessing its general tension and feeling for any tight spots. They will also be looking for tender areas around the outer knee.
2. Obers Test
Obers test is used to assess IT band tightness. The patient is in a side-lying position, with the leg to be tested on top. The therapist will stabilise the pelvis with one hand, whilst they extend the hip with the other. They will then allow the hip to fall down towards the table (abduction). A positive result is noted if the leg moves down less than 10 degrees from horizontal.
As well as these very specific tests, the therapist will probably also look at the range of motion at the hip and knee joints. This will demonstrate how tight the surrounding muscles are, such as the hamstrings, quadriceps and gluteals. These muscles are commonly tight in cases of ITB syndrome.
The therapist should also observe the patient when standing and walking to check if they overpronate.
Subscribe to:
Comments (Atom)